Placemaking for Proximal Health primary care as a common good.

Note: In Placemaking for Proximal Health Part I, we focused on principles of Primary Care.
Ever increasing standards for what it means to be healthy consistently drive the evolution of our healthcare models forward. What has not changed, however, is the critical importance of primary care to the health system at large. Primary care services are undoubtedly an essential strategy for combating the innumerable factors impacting our health. It is a “fact that societies that value primary care also tend to value investment in other collective goods, such as social services, safety nets, and other factors that influence population health” (Stange, Miller, Etz, 2023, p. 813). Prioritizing primary care means leveraging social infrastructure as a platform to make preventative health services accessible and conducive to repeated interactions that build trust in primary care providers.

It is difficult to navigate the modern health system despite the technological advancements of recent years. We often describe the larger health system as complex and fragmented, leaving many frustrated with their healthcare experience. The organization of health systems has undervalued the location of primary care access points within our communities, contributing to physician burnout and an increase in specialized healthcare providers. Ironically, the limited availability of primary care providers in our communities seemingly complicates many individual’s ability to access these specialized providers.
In many cases, finding the right care provider is only half the battle. Today, “80% of U.S. counties are in a healthcare desert,” (Moralez, 2024) a geographic area where there is limited or no access to healthcare. This lack of proximity to healthcare contributes to the limited availability of primary care physicians, especially among rural populations and presents a reality that deserves an innovative response. By leveraging an appreciation for proximal health, communities can begin to mitigate the effects of this barrier by providing social infrastructure that supports primary care services and the relationships they rely on.
ENVISIONING PRIMARY CARE
Understanding health as a synthesis of physical, mental, emotional, spiritual, and environmental factors warrants an expansion of how we envision primary care. The 2021 report “Implementing High-Quality Primary Care: Rebuilding the Foundation of Health Care,” states that “High-quality primary care is the provision of whole-person, integrated, accessible, and equitable health care by interprofessional teams that are accountable for addressing the majority of an individual’s health and wellness needs across settings and through sustained relationships with patients, families, and communities” (Robinson, Meisnere, Philips, et al., 2021). It represents a system that benefits from an effort to reinforce our cultural pursuit of communal well-being through healthy placemaking.
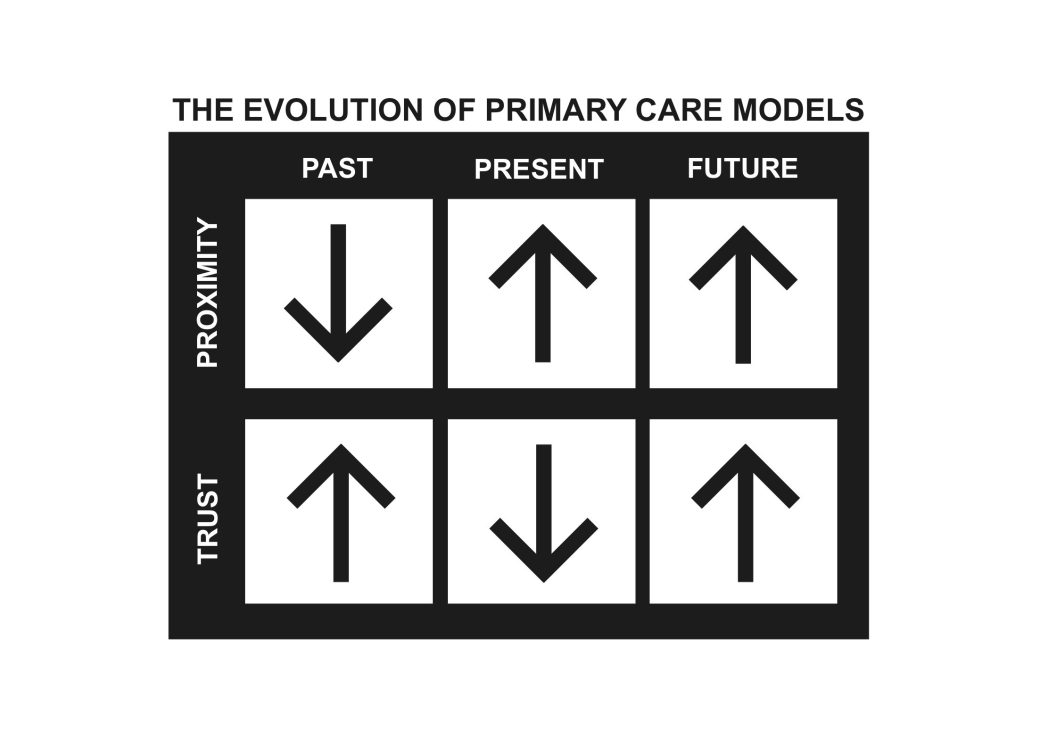
Today, with the ability to receive healthcare both in person and virtually, relationships with primary care physicians can be difficult to maintain. Virtual healthcare models have, in some sense, improved our “proximity” to healthcare providers. Although this approach has improved our access to care, this sort of proximity often lacks familiarity derived from the in-person relationships that are often critical in fostering sustained trust.
A recent publication from Exploring Health describes the danger of depending entirely on virtual healthcare in developing sustained relationships as follows:
“The direction of leveraging telehealth and retail models of primary care has resolved some issues while simultaneously facing others. Considering consumerism in healthcare has allowed patients to drive their own health decisions just as “People are used to shopping online for clothes and shoes. Now they can shop online for their health” (Shah, 2024). This shift has diminished the presence of sustained relationship\s between patients and their physicians resulting in a lower quality of health traded for higher access to it.”
When applied under the right circumstances, telehealth can be leveraged as a powerful tool to maintain our health and sustain patient/provider relationships. First, however, we must create communities conducive to familiar, in-person relationships through placemaking that prioritizes proximal health. By developing right-sized spaces for primary care providers in our communities, we can improve our familiarity and trust in healthcare facilities and providers.
MODELS MOVING FROWARD
The Lutheran Health Physicians (LHP) Primary Care clinic, located on the northeast side of Fort Wayne, is a prototype clinic model focused on centralizing primary care and imaging service lines within communities. Healthcare access points such as this clinic are pivotal in the progression of placemaking for proximal health and the development of trusted provider relationships. It is increasingly important that access to these facilities is provided through effective social infrastructure allowing patients to build relationships with providers and the neighborhood they look to serve.


PROXIMAL PRIMARY CARE
Protecting our health is not the sole burden of primary care; rather our health relies on connectedness to our community, a network that relies on the presence of primary care.
Living in proximity to familiar places and people over time encourages us to build meaningful relationships. Within the context of healthcare, our willingness to trust providers can dramatically benefit from a proximal approach—one that leverages primary care as an integral ingredient to effective, healthy community development.
To improve the effectiveness of primary care, social infrastructure can be harnessed as a model for providing preventative health services by increased proximity and trust in our primary care providers.


